From Discovery to IND: Integrated Support for Cell and Gene Therapy Development

At Inotiv, we help you move confidently from early discovery through IND-enabling development with tailored support for cell and gene therapy (CGT) programs. Whether you're optimizing a novel vector, validating a new target, or preparing for regulatory submission, our multidisciplinary talented team works as an extension of yours—bringing scientific insight, operational excellence, and regulatory awareness to every step.
From efficacy modeling to biodistribution, target gene expression detection, immunogenicity, and GLP toxicology, we deliver the data you need to advance with confidence. Our experience spans a wide range of modalities, including viral and non-viral gene therapies, DNA and RNA based biotherapeutics, genome editing platforms, and autologous or allogeneic cell therapies.
Early-stage innovation deserves expert guidance and execution. At Inotiv, we provide a seamless continuum of services from discovery to first-in-human studies, built on a foundation of science, quality, and partnership.
Partner with experts who understand the science behind your therapy.
At Inotiv, our scientists work closely with you to define study objectives and generate the critical data you need across a range of therapeutic applications, including:
- In vitro discovery and proof-of-concept studies
- Efficacy evaluations
- Non-GLP and GLP toxicology studies in rodents, non-human primates (NHPs), and other large animal models
- Biodistribution and vector shedding assessments
- Target gene expression analysis
- DNA and RNA-based therapeutics
- AAV-related studies
- Cell therapy investigations
Select any scientific area below to discover how partnering with Inotiv accelerates development of your novel therapy.
General Scientific and Technical Frequently Asked Questions (FAQs)
What is the goal of preclinical development in CGT?
To generate data on safety, efficacy, pharmacodynamics (PD), pharmacokinetics (PK), target gene expression quantification, off target detection, persistence, and biodistribution that support initiation of first-in-human clinical trials (usually via an IND or CTA submission).
How do CGT products differ from small molecules in preclinical studies?
CGTs are often species-specific and involve complex biological systems, making standard animal models less predictive. Cell viability, vector delivery, and host immune response are additional variables.
What are common vector platforms used in gene therapy preclinical work?
Adeno-associated viruses (AAV), lentivirus, and non-viral systems like lipid nanoparticles. Selection depends on the target tissue, duration of expression needed, and immunogenicity profile.
In Vivo and In Vitro Model Frequently Asked Questions (FAQs)
What are the challenges in selecting animal models for CGT?
Human cells or vectors may not function as intended in animal systems. This necessitates the use of immunocompromised animals or transgenic/“humanized” models to mimic human disease and biology.
What in vitro studies are essential for CGT preclinical development?
Studies often include:
- Transduction/transfection efficiency
- Cell expansion and phenotype
- Potency assays (mechanism of action)
- Off-target effects (for gene editing)
- Vector genome integration profiling
How is biodistribution assessed?
Using qPCR, in situ hybridization, or imaging, developers track where the vector/cells go post-administration to evaluate safety and predict potential toxicities.
Toxicology and Safety Frequently Asked Questions (FAQs)
What types of toxicology studies are required for CGTs?
Repeat-dose and single-dose toxicity, genotoxicity (for integrating vectors), tumorigenicity (especially for stem cell products), and immunogenicity studies are often needed. Study designs are product-specific.
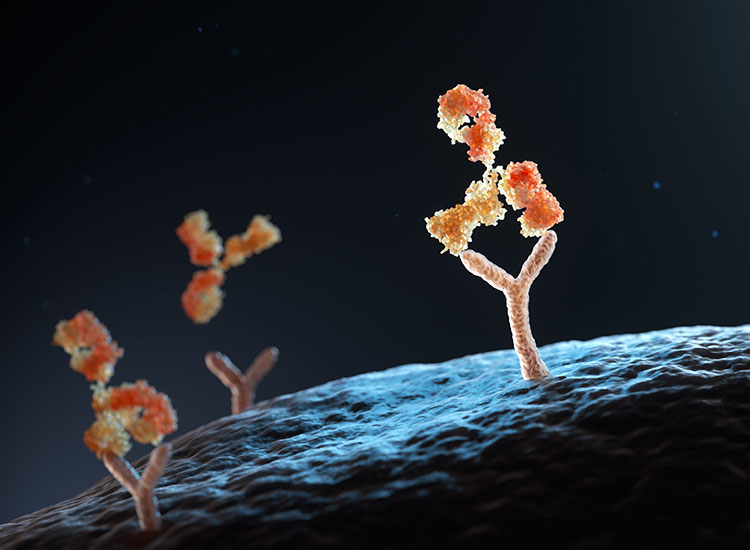
How is immunogenicity evaluated preclinically?
By assessing antibody formation against the vector or transgene, cytokine profiles, and immune cell activation in vitro and in vivo.
Are Good Laboratory Practice (GLP) studies required for IND submission?
Yes. Key toxicology studies that support human dosing must follow GLP standards, particularly those used to define the No-Observed-Adverse-Effect Level (NOAEL).
Regulatory and IND-Enabling Frequently Asked Questions (FAQs)
What are the key components of an IND-enabling preclinical package?
- Proof-of-concept efficacy data in relevant models
- Biodistribution and shedding studies
- Toxicology (GLP-compliant)
- Immunogenicity and tumorigenicity evaluations
- CMC data on test article used
How early should I engage with regulatory agencies like the FDA?
As early as possible. A pre-IND meeting (or INTERACT meeting for novel CGTs) helps align on study design, endpoints, and regulatory expectations.
What are shedding studies, and are they required?
Shedding studies determine if the therapy (especially viral vectors) is excreted from the body via bodily fluids like blood, saliva, urine, feces, semen, nasal secretions and sweat, potentially posing a risk to others. These are typically required for gene therapies.
Emerging and Practical Frequently Asked Questions (FAQs)
What are the biggest pitfalls in CGT preclinical programs?
- Using non-representative animal models
- Inadequate potency assays
- Inconsistent vector/cell production
- Underestimating immunogenicity
- Delaying CMC-regulatory alignment
Can I skip certain studies if I have strong in vitro data?
Not typically. Regulators generally expect both in vitro and in vivo data, though there may be flexibility for well-justified cases or rare diseases with no animal model.
How long does the preclinical phase typically last?
Depending on complexity, 12–24 months from proof-of-concept to IND submission is common, though timelines vary significantly by product type and indication.